Urine, Blood, Breath Ketones: Which is Best?
/Author: Laura Dority MS RD LD
Ketones, ketones, ketones! At every appointment, your keto dietitian is likely asking you about ketones…like a broken record. What is the level? How often are you checking? Do you notice a difference in levels between “good” or “bad” seizure days?
And maybe sometimes you are asking yourself, do ketones really help guide treatment? Are we checking enough? Too much? Are we using the best form of ketone monitoring?
Let’s dig into some of these questions. Please keep in mind that a lot of this blog is going to be strictly my opinion and personal experience with treating ketogenic diet patients. It doesn’t mean that if your keto program does it differently – that it’s wrong!
Are Ketones Important?
The easy answer – yes of course they are! However, you must always keep in mind that the ketogenic diet is treating seizures NOT ketone levels. If someone walks into my clinic with a low level of ketones but not having any seizures, that’s awesome! I’m not going to change anything just because of a low ketone level or trace or even negative. I’m going to make my changes based on seizure control as well as all other clinical data which MAY include the ketone level!
Some forms of ketogenic diet therapy – looking at you low glycemic index treatment –don’t even produce ketones in certain patients. Something to keep in mind!
Overall for most patients ketones are important but are not the end all be all.
What is the Ideal Ketone Level?
It’s 100% individualized. I have patients that do fantastic at a small ketone level while I have other patients that absolutely have to be in the large range. Why the difference? It’s really hard to say – maybe related to the specific cause of the epilepsy? Age? Weight? Metabolism? Thankfully researchers are looking into this exact question!
I certainly have some patients that need to be at a specific ketone level to have ideal seizure control. I have seen this situation specifically with GLUT 1 deficiency patients and Dravet Syndrome. Based on my observations these 2 subgroups of the epilepsy population tend to do best at higher levels of ketones.
While I have other patients that the level of ketones do not seem to directly correlate with seizure control. For example, they may have a “good” seizure day at small ketones and then a “bad” seizure day with large ketones one week and then it completely flip-flops the next week.
What is the Best Way to Check Ketones?
There are three different ways to check ketone levels – each actually measuring a different ketone body. Let’s learn more about each and when I may recommend one over the other.
Option 1: Urine ketones
Measures acetoacetate
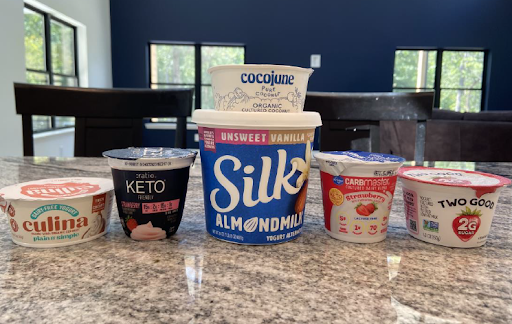
Generally measured in trace, small, moderate or large but can also have a number associated with the reading (see photo above)
Trace = 5 mg/dL
Small = 15 mg/dL
Moderate = 40 mg/dL
Large = 80-160 mg/dL
Advantages:
Inexpensive
Simple
Non-invasive
Many different brands (including available on Amazon)
Disadvantages:
Least accurate
Shows the ketone level that WAS available for use (past by-product not a real time test)
Impacted by hydration and other factors
Option 2: Blood ketones
Measures betahydroxybutyrate
Recommended brand: Keto MoJo
Company has excellent customer service, how-to resources, and FAQ on website.
Advantages:
Dual glucose/ketone meters available
More accurate
Levels are reflected in real time
Not impacted by hydration
Disadvantages:
Potentially more expensive (cost of strips have decreased from $0.99/each to $0.80/each with the newest meter model)
Lack of insurance coverage (newest meter may be eligible for FSA and HSA)
Involves finger prick which can be painful and traumatic for some children
Option 3: Breath ketones
Measures acetone
Has been around for >100 years but not widely used in the epilepsy world at this time
Recommended brand: Keyto
Advantages:
Non-invasive
Simple
Disadvantages:
Expensive (one-time cost versus daily strips with blood meteres)
Lack of insurance coverage
Personally I do not have any experience using breath ketone meters in my patients, but I did find this article that was interesting and helpful.
In my opinion, urine ketones are a good option for many of my patients who don’t need a very specific level of ketosis. For example a child that does well regardless if ketones are small or large versus a child who needs to be within a very specific ketone range of say 5-6 mmol/L depicted in blood levels.
Patients with a consistent intake of water (g-tube fed kids for example) who get the exact same fluid and formula intake every day are also good candidates for urine ketones. In these situations, the variability of hydration isn’t a factor.
On the other hand, patients that really need to be at a specific ketone level for seizure control may need a blood meter. Many of my GLUT 1 Deficiency Syndrome and Dravet Syndrome patients have meters for this exact reason.
And finally, the reality is that cost can play into my decision! In most cases I’m already asking families to pay for supplements, a gram scale, specialized formula and food so if insurance will not cover a blood meter then urine ketones may be my only option.
When I do have families measuring urine ketones in the home environment, I certainly do check their blood level in clinic every 3-6 months. From a cost perspective this does allow insurance to hopefully cover the lab draw and usually provides frequent enough information to tweak their keto plan appropriately.
Utilizing both urine levels at home and blood levels from the lab can help you look at the big picture without unnecessarily pricking the child. Because the reality is we are already asking these children to eat a restricted diet – unique from their peers- and now we want them to prick their fingers on a regular basis? I certainly know kiddos that wouldn’t bat an eye at pricking their finger and then I also know children that it completely traumatizes them. It’s a balance between getting the best data to guide treatment but also not causing pain or trauma if we don’t have too. Maybe that is where breath ketone meters really can play a role in the future!
Overall, there isn’t a right or wrong – I have keto colleagues that only do blood meters while I have other keto colleagues that only do urine ketones. Beth Zupec-Kania, RDN, CD wrote a great blog titled “Checking for Ketones” a few years ago for the Charlie Foundation for Ketogenic Therapies that would be a great read to get another perspective on this topic.
When Should You Check Ketones?
Easy answer- however often your keto team tells you too! Seriously, they know your kiddo better than me writing this general blog on ketone levels!
My thought process for my patients involves the following questions:
How old is the child?
How easy is it to obtain ketone levels (in other words- let’s not traumatize the small humans)?
How much variability is in the diet?
What form of ketone monitoring (blood vs urine) are we using?
Generally, if I have a patient starting the diet I will ask for daily ketone levels so I can evaluate the transition into ketosis. On the other hand, for those kiddos who are stable and have minimal variety in their diet (for example kids on g-tube feeds), then weekly levels are adequate.
Checking ketones during times of increased seizure activity may also be helpful. Scenario – A child who is normally in large ketones with good seizure control randomly has a dramatic increase in seizures. Parents check a ketone level and find the level is abnormally small. We can then go back and brainstorm any changes over the past few days to identify what potentially decreased the ketone levels and prevent in the future. We can also adjust the diet to get the ketones boosted quickly back to the large range.
So at your next keto appointment when your RD and MD ask you – what have your ketone levels been……? Now you know that this is a loaded question and not as black and white as we would hope! If your team is asking you to check your ketone levels X times a week or month – please do so. The ketone level can provide good clinical insight and guide changes to the diet to better help your child’s seizure control.
Disclaimers:
Insurance coverage of ketone monitoring supplies will vary largely from state-to-state and insurance companies.
We are not affiliated with nor did we receive any funding from ketone monitoring companies for this blog.
This blog is not intended to be medical advice. This is strictly one ketogenic dietitians’ opinion. Please always follow your ketogenic diet teams instructions for all aspects of your ketogenic diet including ketone monitoring.